Articles
- Page Path
- HOME > Perspect Integr Med > Volume 3(1); 2024 > Article
-
Editorial
A Pilot Trial of Integrative Medicine for Stroke Rehabilitation: Expert Recommendations for the Development and Sustainability of Integrative Medicine -
Chihyoung Son1
 , Go-Eun Lee1
, Go-Eun Lee1 , Joo-Hee Seo2
, Joo-Hee Seo2 , Inae Youn2
, Inae Youn2 , Jin-Won Kim2,*
, Jin-Won Kim2,*
-
Perspectives on Integrative Medicine 2024;3(1):1-6.
DOI: https://doi.org/10.56986/pim.2024.02.001
Published online: February 22, 2024
1Department of Korean Medicine Rehabilitation, National Rehabilitation Hospital, Seoul, Republic of Korea
2Department Korean Traditional Medicine, National Medical Center, Seoul, Republic of Korea
- *Corresponding author: Jin-Won Kim, Department of Korean Traditional Medicine, National Medical Center, Eulgiro 245, Seoul 04564, Republic of Korea, Email: sandman6354@gmail.com
©2024 Jaseng Medical Foundation
This is an open access article under the CC BY-NC license (http://creativecommons.org/licenses/by-nc/4.0/).
- 653 Views
- 17 Download
Abstract
-
Background
- Strategies towards development and sustainability of integrative treatment in stroke rehabilitation medicine are needed. National expert recommendations based on the implementation of Integrative Medicine (IM) in stroke rehabilitation and IM outcomes would be invaluable.
-
Methods
- A pilot study was performed and the effectiveness of combining Korean traditional medicine and Western conventional medicine in post-stroke patients (ischemic stroke n = 15 and hemorrhagic stroke n = 4) was evaluated, and recommendations were developed through consensus with physicians in national centers of rehabilitative medicine. Outcome measures [Korean Modified Barthel Index (K-MBI), Korean Mini Mental State Examination (K-MMSE), Modified Rankin Scale (mRS), and EuroQol 5-dimension 5-level (EQ-5D-5L) assessment were used at baseline, 4, 8 (K-MBI, K-MMSE, mRS, and EQ-5D-5L) and 12 weeks post treatment (EQ-5D-5L and mRS).
-
Results
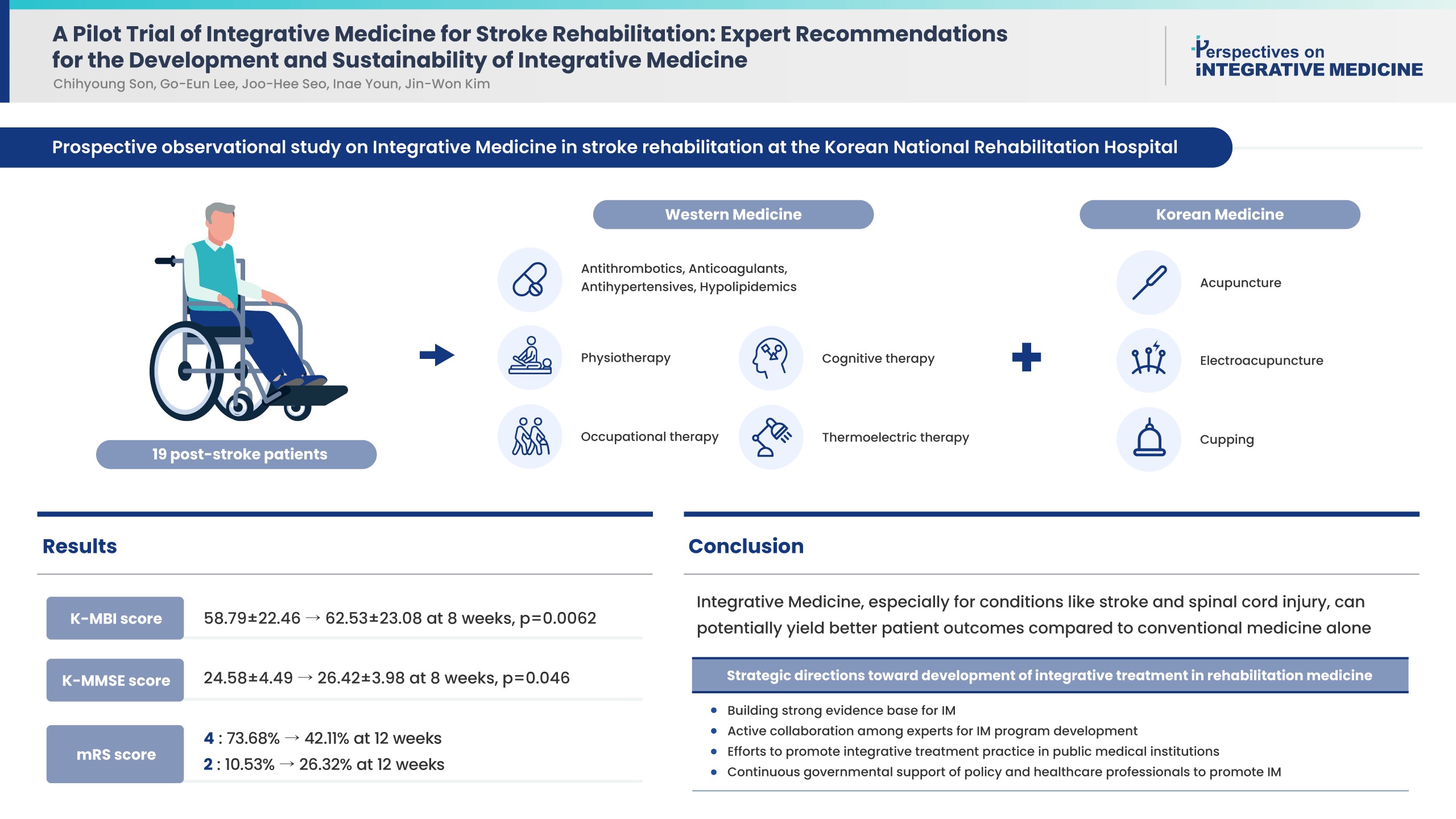
- Improvements were observed in functional and cognitive abilities at 8 weeks (K-MBI score p = 0.0062; K-MMSE score p = 0.046). Quality of life improvements (EQ-5D-5L) were observed but were not statistically significant. The disability assessment (mRS) indicated a gradual improvement from baseline to 12 weeks. No adverse events were reported. For effective, patient-centered IM treatment: (1) build a strong evidence base for IM as compared with Western medicine alone or traditional medicine alone; (2) active expert collaboration; (3) IM promotion in public medical institutions; and (4) continued government support.
-
Conclusion
- Functional and cognitive abilities of stroke patients statistically significantly improved following 8 weeks of IM treatment. Strategies have been suggested towards the development and sustainability of IM treatment in stroke rehabilitation medicine.
- Integrative medicine (IM) incorporates Korean traditional medicine that is evidence-based, natural, and complementary (along with lifestyle interventions) into evidence-based Western conventional medicine to provide comprehensive patient-centered care [1]. The practice of IM is based on the practitioner-patient relationship, and addresses the individual’s holistic well-being, relying on evidence-based practices, and incorporating a wide range of therapeutic modalities, healthcare professionals, and disciplines to achieve optimal health and healing [2].
- In Korea’s healthcare system, both Western conventional medicine and Korean traditional medicine are practiced under a dual medical system [3], and there has been government efforts to develop the dual system into a system of IM that considers each patient’s unique background and characteristics. Since 2010, statutory reform allowed Western conventional medicine hospitals to hire Korean traditional medicine doctors to provide institutional support for the development of an integrated system.
- As part of the strategy towards the development of an IM system, national hospitals such as the National Medical Center and National Rehabilitation Center (NRC) in Korea established Departments of Korean traditional medicine that integrate collaborative Korean medicine-Western medicine (KM-WM) treatments. The NRC, which is run by the Ministry of Health and Welfare, serves as a specialty rehabilitation center, undertakes research, and programs for people with disabilities, alongside operating a specialty rehabilitation hospital. The NRC provides rehabilitation to post-stroke patients, those with spinal cord injury, and those with other conditions, and runs an intensive inpatient rehabilitation program. The NRC has provided Korean traditional medicine along with Western conventional medicine since December 2010 with the aim of practicing IM.
- A number of clinical practice guidelines have mentioned integrative treatments such as acupuncture, as a post-stroke management option [4], but specific recommendations vary by guidelines depending on the evidence used for generating guidelines. This presents a gap between the recommendations and clinical practice in the real-world setting in Korea, where rehabilitation treatments involving acupuncture is provided to post-stroke patients.
- Here, we present our experience (process and outcomes) providing IM treatment at a national hospital with the aim of achieving the best patient outcomes. We investigate whether the physical function and quality of life (QoL) of patients improved following IM treatment for patients undergoing stroke rehabilitation. Based on this experience, the opinions of experts in IM at national hospitals was collated to propose sustainable strategies for implementing IM in the field of rehabilitation medicine.
Introduction
- A single-arm prospective observational study was conducted at the Korean National Rehabilitation Hospital in Seoul from October 2016 to September 2017. The study was approved by the Institutional Review Board (no.: NRC-2016-05-042) and was registered with the Clinical Research Information Service (no.: KCT0002263). All participants provided written informed consent for the study.
- Patients admitted to hospital for stroke (cerebral infarction, cerebral hemorrhage) who underwent integrative KM-WM treatments and who provided written informed consent were enrolled in the study. The inclusion criteria were as follows: (1) stroke patients receiving KM-WM integrative treatment; (2) aged ≥ 19 years; (3) and the ability of patient or caregiver to communicate effectively. The exclusion criteria were as follows: (1) currently pregnant or breastfeeding; (2) had participated in other clinical trials within the last 30 days; and (3) deemed unsuitable for this study by the researchers.
- 1. Intervention
- The participants were treated with KM-WM simultaneously. The participants were prescribed Western medicines such as antithrombotics, anticoagulants, antihypertensives, and hypolipidemics. They were also treated with physiotherapy and occupational therapy more than 5 times per week. Some patients received cognitive therapy (twice per week) or thermoelectric therapy (5 times per week). Korean traditional medicine therapy for stroke such as acupuncture, electroacupuncture, and cupping was performed 2 or 3 times per week by Korean traditional medicine doctors who had been educated for 6 years at a medical university teaching traditional Korean medicine and who had engaged in medical practice for at least 4 years.
- The Korean Modified Barthel Index (K-MBI) [5], Korean Mini Mental State Examination (K-MMSE) [6], Modified Rankin Scale (mRS) score [7,8], and EuroQol 5-dimension 5-level (EQ-5D-5L) assessment [9,10] were used to assess the participants. All outcomes were assessed at baseline and after 4 and 8 weeks of treatment, while EQ-5D-5L and mRS were additionally assessed after 12 weeks of treatment. Adverse events were also evaluated.
- An intention-to-treat analysis was performed. Missing data were imputed using the last observation carried forward method. Descriptive analysis covered the participants’ sociodemographic variables and stroke characteristics. Scale changes were analyzed using paired t tests or the chi-square tests. The changes in K-MBI and K-MMSE from baseline to 8 weeks were analyzed in detail by age and onset using an independent t test. Data are presented as mean ± SD, the 95% confidence interval was used for quantitative data, and numbers and percentages were used for categorical data. Significance was set at p < 0.05 for 2-tailed tests. Stata/SE Version 12.0 was used for the analysis.
- 2. Results
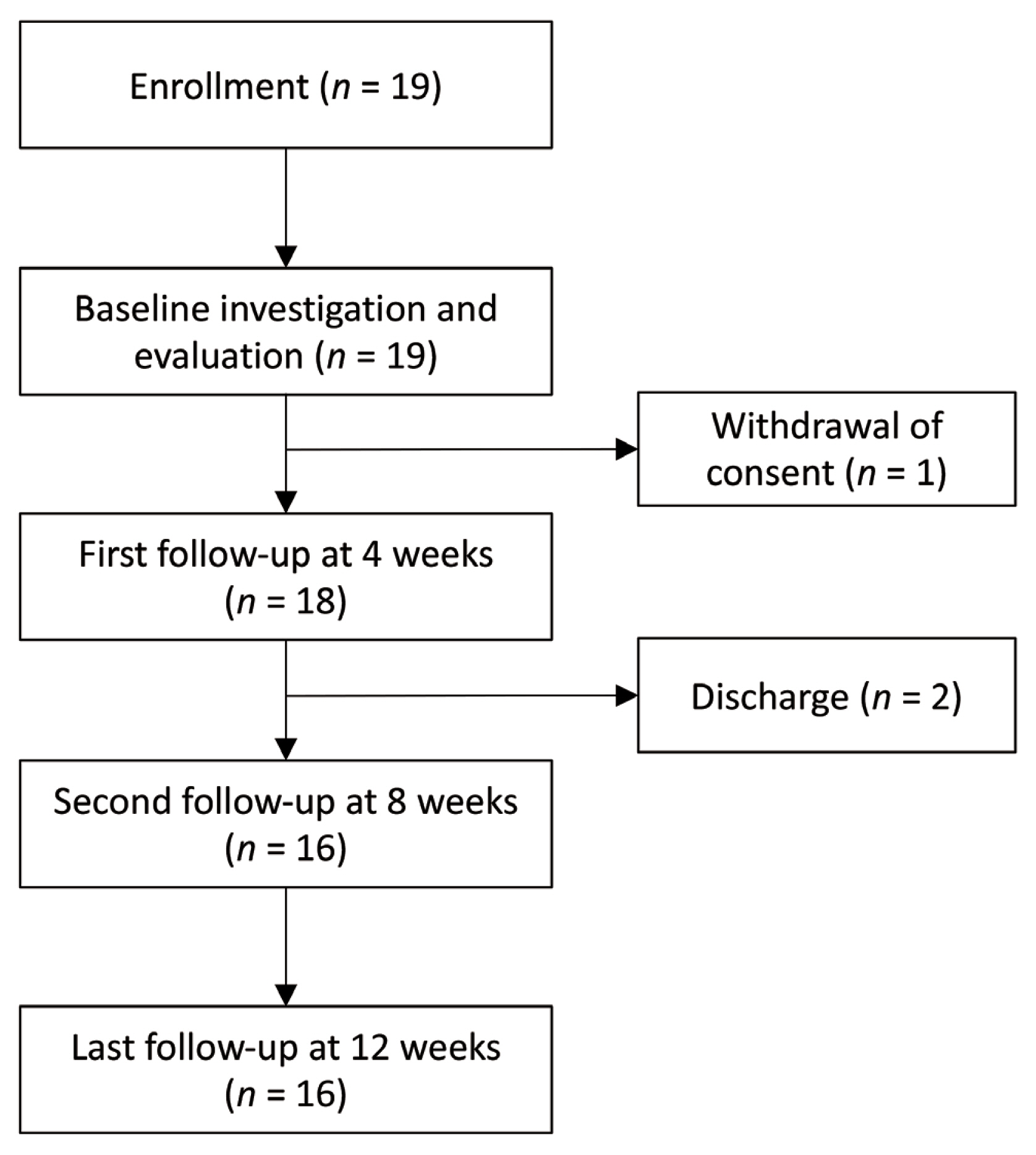
- A total of 19 patients were enrolled in this study (Fig. 1); of these, 16 finished their follow-up. One participant withdrew consent after the baseline examination, while 2 participants dropped out after 4 weeks of treatment at hospital discharge. None of the participants dropped out due to illness or worsening symptoms.
- The average participant age was 65.63 ± 6.49 years, and the population included 9 men (47.37%) and 10 women (52.63%; Table 1). Among the participants, 15 (78.95%) had ischemic stroke and 4 (21.05%) had hemorrhagic stroke. The duration from the onset of stroke to enrollment was 123.53 ± 74.08 days, and 8 patients (42.11%) experienced the onset within 3 months of starting the trial. Regarding the National Institutes of Health Stroke Scale scores, 9 had a score of ≤4, whereas 10 had scores of 5–20. Videofluoroscopic swallow study reports were available for 5 (26.32%) patients.
- The mean K-MBI score improved significantly from 58.79 ± 22.46 at baseline to 62.53 ± 23.08 at 8 weeks (p = 0.0062). The mean K-MMSE score decreased significantly from 24.58 ± 4.49 at baseline to 26.42 ± 3.98 after 8 weeks of treatment (p = 0.046). Changes in the EQ-5D-5L scores indicated an improved QoL of patients from 0.43 ± 0.22 at baseline to 0.44 ± 0.18 at 8 weeks to 0.47 ± 0.18 at 12 weeks, but the differences were not statistically significant. Patients with the mRS score of 4 accounted for 73.68% at baseline and 42.11% at 8 and 12 weeks, while those with the mRS score of 2 accounted for 10.53% at baseline, 21.05% at 8 weeks, and 26.32% at 12 weeks, indicating a gradual improvement over time. The changes in the main outcomes are presented in Table 2. No adverse events were reported during the study.
- 3. Study implications and limitations
- This single-arm observational study aimed to investigate the characteristics, changes in physical and mental function, changes in QoL, and hospitalization of stroke patients who experienced KM-WM collaborative treatments. This is a preliminary study whose findings may aid the planning of more advanced studies in IM for stroke rehabilitation.
- A Cochrane review of acupuncture for stroke rehabilitation reported evidence that acupuncture may improve independency and neurological deficiencies after stroke [11]. A systematic review reported that acupuncture effectively treated neurological impairment and dysfunction after stroke [12]. However, studies related to acupuncture or traditional medical treatments for stroke have previously been criticized for their low quality [13,14]. Another systematic review of the clinical benefits of integrated Western conventional medicine and Chinese traditional medicine for stroke rehabilitation reported that IM was superior when dependency and swallowing function was evaluated compared with the standard Western conventional medicine therapy alone; however, this review also pointed out that most of the included studies were short in duration (2–4 weeks) [15]. In comparison, the current study was a long-term (8-week) observational study that reported the experience and outcomes of implementing IM treatment for inpatients at a national hospital in Korea. However, our pilot study did not include control groups to enable a comparative analysis, and since it included a small sample of 19 patients, it is not possible to generalize the findings to all populations.
Experience from a Pilot Study on IM Treatment for Stroke Rehabilitation in a National Hospital in Korea
- Based on the experience from this pilot study, discussions were held to reach a shared consensus among physicians in the national medical centers of rehabilitative medicine in Korea to generate suggestions for a strategic sustainable direction for IM treatment. The following steps are proposed to promote the development of IM treatment in rehabilitation medicine (Table 3).
- 1. Building strong evidence base for IM
- The first step in the development of a sustainable integrative treatment practice is the accumulation of evidence, without risk of bias, demonstrating its safety, and efficacy in its outcomes. The primary goal of IM is to improve patient outcomes. In this context, it is imperative to collect evidence about how IM improves patient outcomes. In addition, in the future, more evidence needs to be accumulated about its efficacy and safety, and it will be necessary to consider aspects other than functional improvement or QoL.
- 2. Active collaboration amongst experts for IM program development
- Secondly, a mutual understanding is required between experts in Western conventional medicine doctors and Korean traditional medicine doctors. The lack of a mutual understanding makes it difficult to identify areas of medicine that would benefit from IM program establishment. Western conventional medicine and Korean traditional medicine professionals must recognize that the common goal is to provide effective, patient-centered IM treatment. The efficiency of IM treatment provided without such collaborations will decrease. Accordingly, patients may believe that IM treatment requires treatments from experts in 2 fields rather than 1, and may think IM treatment will result in a longer treatment duration. To prevent such consequences, the efficient implementation of IM treatment requires an enhanced degree of mutual understanding and active collaboration.
- 3. Efforts to promote integrative treatment practice in public medical institutions
- Since public medical institutions tend to be more likely to encourage collaboration than private medical institutions, they may be in better positions to establish a patient-centered system of IM treatment. As presented in this pilot study, public institutions may propose the development of IM treatment protocols for other critical illnesses such as cancer and subsequently disseminate these protocols to private hospitals. However, since IM treatment is not actively implemented for many other conditions than stroke rehabilitation in national public hospitals therefore, government-level strategic support will be required.
- 4. Continuous governmental support of policy and healthcare professionals to promote IM
- To enable continued and expanded implantation of IM, support in terms of related institutions and human resources is necessary. A pilot KM-WM project is currently underway in Korea. Starting in 2016, the Korean government has supported research to collect evidence of efficacy in KM-WM collaborative treatments for the establishment of the Monitoring Center for Korean Medicine and Western Medicine Collaboration [16]. In this project, when Western conventional medicine and Korean traditional medicine treatments are provided on the same day under the same disease code in a collaborative outpatient environment, health insurance coverage is granted for both practices. Moreover, for several specific diseases, a fee for the collaborative consultation is provided, thereby promoting the joint endeavor. However, in real-world practice, to expect the active implementation of collaborative treatment is farfetched due to limited availability of adequate incentives to motivate the physicians, who are partners in collaborative treatment, to take initiative. Therefore, if Korea is planning to establish an IM treatment system in the future, providing continuous institutional and financial support to national hospitals, which tend to experience less inter-professional conflict than private hospitals, would be helpful.
- Support which promotes effort towards the development of the IM treatment program, as well as the active accumulation and presentation of related evidence, would be beneficial. Furthermore, the development of outcome measures that would effectively reflect the benefits of IM treatment is necessary.
- For conditions and diseases involving irreversible states such as spinal cord injury or stroke, whose rehabilitation benefits only to a degree by Western conventional medicine treatment alone, IM treatment may achieve better patient outcomes. The findings of this study suggest a promising outlook for IM in the field of stroke. Based on the suggestions discussed above, a more sustained effort should be made to ensure the future of IM development.
Recommendations for Strategic Directions Towards the Development of Integrative Treatment in Rehabilitation Medicine
-
Author Contributions
This research was conducted by all authors. Conceived the study: JWK, CHS, GEL, and JHS. Drafted the manuscript and designed the observation protocol: IAY, JWK, CHS, and GEL. Managed the participant schedule and data: CHS. Evaluated the assessment tools: GEL. Prepared the manuscript CHS, JWK, and IAY. Reviewed the manuscript: GEL and SJC. All authors read and approved the final manuscript for submission.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
This study was supported by the Ministry of Health and Welfare of Korea (no.: 3234-302).
-
Ethical Statements
This single-arm prospective observational study was conducted at the Korean National Rehabilitation Hospital in Seoul from October 2016 to September 2017. The study was approved by the Institutional Review Board (no.: NRC-2016-05-042) and registered with the Clinical Research Information Service (no.: KCT0002263). All participants provided written informed consent for the study.
Article information
| Baseline | 4 wk | 8 wk | 12 wk | ||
|---|---|---|---|---|---|
| K-MBI | 58.79 ± 22.46 (47.96, 69.61) | 61.42 ± 24.28 (49.72, 73.12) | 62.53 ± 23.08 (51.40, 73.65) | - | |
| Difference | −2.63 ± 4.06 (−4.59, −0.68) | −3.74 ± 5.26 (−6.27, −1.20) | - | ||
| p | 0.0112* | 0.0062* | - | ||
|
|
|||||
| K-MMSE | 24.58 ± 4.49 (22.42, 26.74) | 25.42 ± 4.23 (23.38, 27.46) | 26.42 ± 3.98 (24.50, 28.34) | - | |
| Difference | −0.84 ± 1,74 (−1.68, −0.003) | −1.84 ± 3.75 (−3.65. −0.04) | - | ||
| p | 0.0492* | 0.046* | - | ||
|
|
|||||
| EQ-5D-5L | 0.43 ± 0.22 (0.33, 0.54) | 0.45 ± 0.21 (0.35, 0.55) | 0.44 ± 0.18 (0.35, 0.53) | 0.47 ± 0.18 (0.39, 0.55) | |
| Difference | −0.18 ± 0.04 (0.15, −0.92) | −0.10 ± 0.04 (−0.08, 0.06) | −0.37 ± 0.03 (0.14, −0.10) | ||
| p | 0.6169 | 0.7769 | 0.2615 | ||
|
|
|||||
| mRS score (%) | 2 | 2 (10.53) | 3 (15.79) | 4 (21.05) | 5 (26.32) |
| 3 | 3 (15.79) | 4 (21.05) | 7 (36.84) | 6 (31.58) | |
| 4 | 14 (73.68) | 12 (63.16) | 8 (42.11) | 8 (42.11) | |
* p < 0.05.
EQ-5D-5L = EuroQol 5-dimensions 5 levels; K-MBI = Korean modified Barthel index; K-MMSE = Korean mini mental state examination; mRS = modified Rankin scale.
Data are shown as mean ± SD (95% confidence interval) or n (%) as appropriate, and were analyzed by the independent t test (*p < 0.05).
- [1] Hunter J, Harnett JE, Chan W-JJ, Pirotta M. What is integrative medicine? Establishing the decision criteria for an operational definition of integrative medicine for general practice health services research in Australia. Integr Med Res 2023;12(4):100995. ArticlePubMedPMC
- [2] Maizes V, Rakel D, Niemiec C. Integrative medicine and patient-centered care. Explore 2009;5(5):277−89.ArticlePubMed
- [3] Park HL, Lee HS, Shin BC, Liu JP, Shang Q, Yamashita H, et al. Traditional medicine in china, Korea, and Japan: a brief introduction and comparison. Evid Based Complement Alternat Med 2012;2012:429103. ArticlePubMedPMCPDF
- [4] Birch S, Robinson N. Acupuncture as a post-stroke treatment option: a narrative review of clinical guideline recommendations. Phytomedicine 2022;104:154297. ArticlePubMed
- [5] Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean version of modified barthel index (k-mbi): multi-center study for subjects with stroke. J Korean Acad Rehabil Med 2007;31(3):283−97. [in Korean] https://koreascience.kr/article/JAKO200710103420681.page.
- [6] Kang YND, Hahn S. A validity study on the Korean mini-mental state examination (K-MMSE) in dementia patients. J Korean Neurol Assoc 1997;15(2):300−8. [in Korean] https://www.jkna.org/journal/view.php?number=4088.
- [7] Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke 2007;38(3):1091−6.ArticlePubMed
- [8] Saver JL, Filip B, Hamilton S, Yanes A, Craig S, Cho M, et al. Improving the reliability of stroke disability grading in clinical trials and clinical practice: the Rankin focused assessment (RFA). Stroke 2010;41(5):992−5.ArticlePubMedPMC
- [9] Kim S-H, Jo M-W, Ahn J, Shin S, Ock M, Park J, et al. The valuation of EQ-5D-5L health states in Korea. Value Health 2014;17(7):A753. Article
- [10] Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20(10):1727−36.ArticlePubMedPMCPDF
- [11] Yang A, Wu HM, Tang JL, Xu L, Yang M, Liu GJ. Acupuncture for stroke rehabilitation. Cochrane Database of Syst Rev 2016;2016(8):CD004131. ArticlePubMedPMC
- [12] Park J, Hopwood V, White AR, Ernst E. Effectiveness of acupuncture for stroke: a systematic review. J Neurology 2001;248(7):558−63.ArticlePDF
- [13] Chen X, Mo C, Lu L, Gao R, Xu Q, Wu M, et al. Methological quality of systematic reviews and meta-analyses on acupuncture for stroke: a review of review. Chin J Integr Med 2017;23(11):871−7.ArticlePubMedPDF
- [14] Xue CC, Zhang AL, Greenwood KM, Lin V, Story DF. Traditional Chinese medicine: an update on clinical evidence. J Altern Complement Med 2010;16(3):301−12.ArticlePubMed
- [15] Linda LDZ, Ya Z, Alexander YL, Norman W, Liang Y, Xingyao W, et al. Would integrated Western and traditional Chinese medicine have more benefits for stroke rehabilitation? A systematic review and meta-analysis. Stroke Vasc Neurol 2022;7(1):77−85.ArticlePubMedPMC
- [16] Jun E, Lee H, Cho M, Kim N, Lee I. Trend analysis of Korean-western medicine collaboration studies by disease group. J Int Korean Med 2020;41(4):658−67. [in Korean].ArticlePDF


 PubReader
PubReader ePub Link
ePub Link Cite
Cite


